What is inherited retinal dystrophy?
A collection of rare inherited diseases that affect the retina and causes vision loss.
It looks like you are using an older version of Internet Explorer which is not supported. We advise that you update your browser to the latest version of Microsoft Edge, or consider using other browsers such as Chrome, Firefox or Safari.
A collection of rare inherited diseases that affect the retina and causes vision loss.
As a family member, friend, or a caregiver of someone with an IRD, getting your head around what IRD means will help you to support the individual’s understanding of their condition. Receiving a diagnosis can be a highly emotional experience, and they may struggle to take information in. This website can prepare you, so that you can be on hand to help.
So, what is IRD?
IRD is used to describe a collection of rare eye conditions. IRDs can also be referred to as inherited retinal diseases or inherited retinal degenerations.1
There are lots of different types of IRD. Some names of the more common ones are retinitis pigmentosa (RP), Usher syndrome, Leber congenital amaurosis, and Stargardt disease, all of which you can find more information on here
People with IRD have a mutation in one or more of the genes responsible for the function of the light-sensitive (photoreceptor) cells in the retina at the back of your eye. In IRD these cells begin to lose function or die, which leads to a gradual loss of vision and blindness.1
IRD can affect people at any age but it is a leading cause of vision loss in people of working age (15 to 45 years), and a common cause of visual impairment in childhood. It has been estimated that IRD affects more than 2 million people worldwide (about 1 in every 2000).2
As there are so many different types of IRD, while they affect the vision symptoms and progression are all different.
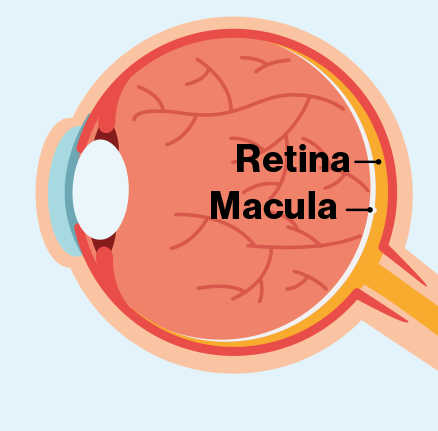
Retina: the back surface of the eye made up of two layers, full of cells that detect light (photoreceptor cells) and send signals to the brain to create images. Contains two types of photoreceptor cells: rods and cones1
Macula: the most light-sensitive part of the retina, densely packed with photoreceptor cells, a central spot that is responsible for colour vision
Rod cells: mostly found around the edge of the retina, these cells are the ones that work in dim light and that help us see things that aren’t straight ahead1
Cone cells: these are concentrated in the centre of the retina and are the cells that are mostly involved in seeing colour and that give us detailed vision1
Learning about IRD in more detail can equip you with a better understanding in order to support the person coming to terms with their diagnosis. You may wonder about the link between gene mutations and IRD. The information below will provide an explanation.
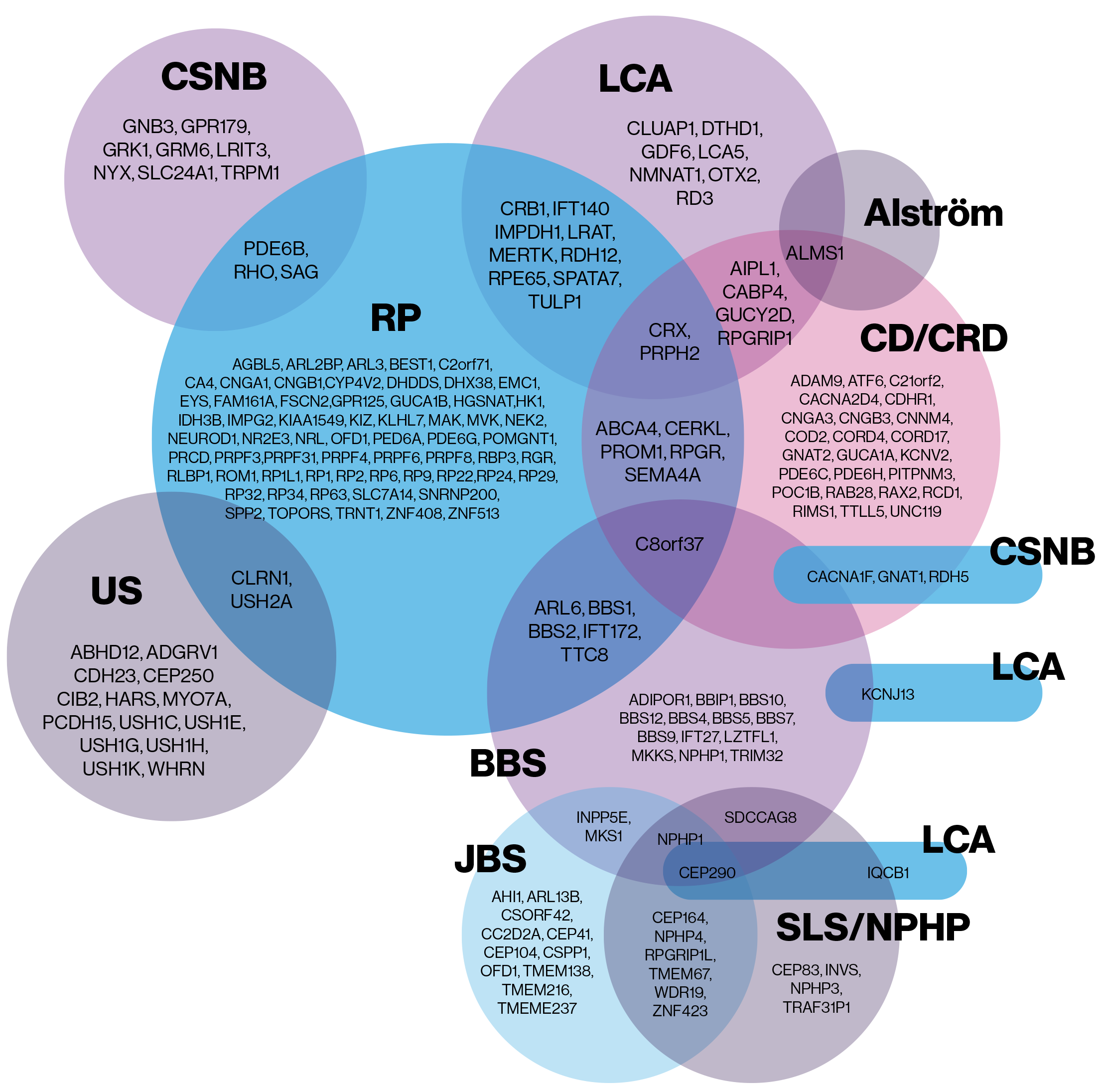
All inherited retinal dystrophies are caused by mutations in genes. These genes are involved in the development and function of light-sensitive cells (photoreceptors) and other cells in the retina.1 More than 260 genes have been associated with IRD, which are thought to cause 60 to 70% of all cases.3,4
Some types of IRD are caused by a single mutation in an identified gene, whereas others can be caused by lots of different mutations but are known by the same name.2 For example, Stargardt disease is usually caused by a mutation in a gene called ABCA4, whereas we know of mutations in 84 different genes that can cause retinitis pigmentosa.2
In some cases the genetic mutation that causes an IRD isn’t yet known, but research is always being done to discover more. Genetic testing can confirm a genetic basis for the disease your child or loved one has and determine what mutation is responsible, how this might affect their progress, and what the likelihood is of passing it on to children of their own.
Common genetic terms
Medical language can feel very jargon-heavy and full of words you may not understand. Here are some of the most common words with quick definitions to make things easier.
You may wonder how IRDs are passed on in families. Different types of IRDs have different inheritance patterns depending on the type of mutation and the gene(s) affected. Below are the different ways that mutations that cause IRD can be inherited.

There are a lot of different conditions that together are called IRDs, many named after the person who first described them. They can be caused by a mutation in one of over 260 genes that have been linked to the conditions and can develop at different ages depending on the type.3
IRDs can be described as syndromic or non-syndromic. Syndromic IRDs are ones in which the eye problems are associated with other symptoms (such as hearing loss in Usher syndrome) as part of a systemic disease, whereas non-syndromic IRDs don’t have these systemic symptoms.6
Some of the more common ones are described below. Other types of IRD can include – Bardet–Biedl syndrome, Joubert syndrome and primary ciliary dyskensia (among others).7
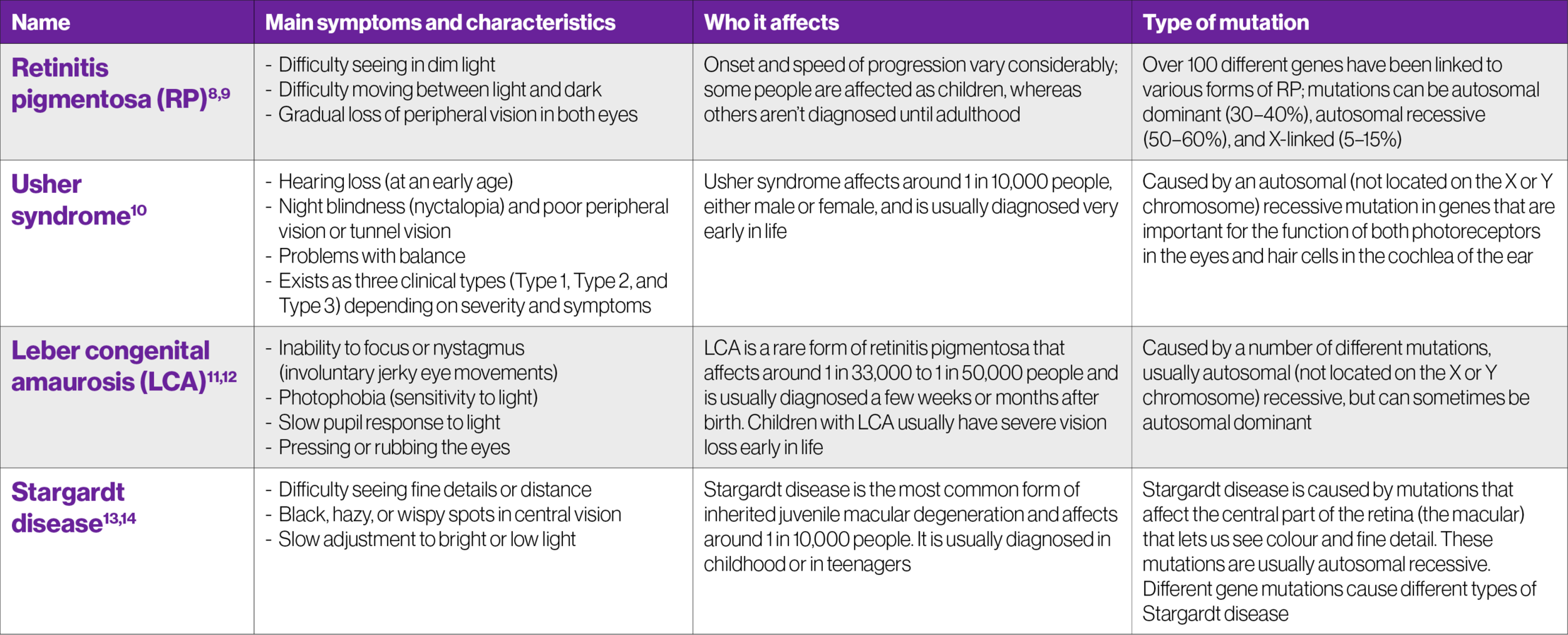
The thought of a condition progressing can be unsettling for both you and the person you are caring for. But knowing the facts and what to expect can put you both at ease and help you plan for the future. How quickly an IRD is likely to progress and what symptoms they will develop can depend on what form and mutation a person has. Even the same IRD can progress differently in different people.
Many conditions start with difficulty seeing in low light levels, before leading to further vision problems. Loss of vision can be slow and gradual or can happen more suddenly. The different examples of visual impairment below help you to understand how the disease can develop.

Tunnel vision or loss of peripheral vision

Spots in the centre of vision

Blur in the centre of vision
Although their vision may worsen, there are a number of things you can do to help the person you are caring for adjust and make changes so that IRD doesn’t stop either of you from living your lives. See more in our section on Support and resources
IRD can progress differently in different people, and so it’s important to get the most accurate diagnosis you can. For more information on clinical diagnosis and genetic testing click here
_________________